The healthcare industry is evolving rapidly, making medical billing and coding an essential function for any medical practice. An efficient medical billing and coding company ensures smooth revenue cycles, reduces claim denials, and allows healthcare providers to focus on patient care. However, with so many companies in the market, choosing the right one can be a challenge. In this blog, we’ll outline the key factors to consider when selecting a medical billing and coding company for your practice.
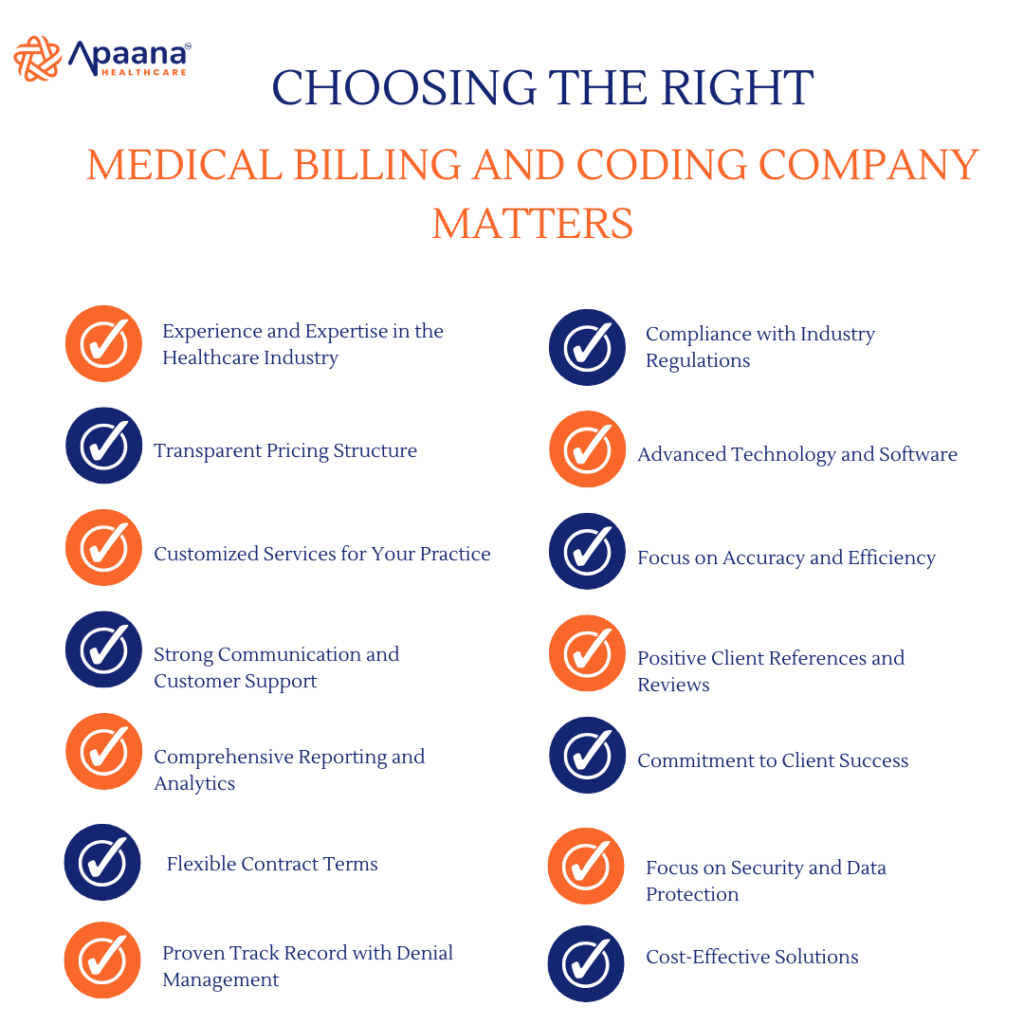
Why Choosing the Right Medical Billing and Coding Company Matters
A reliable medical billing and coding company does more than handle claims—it ensures financial stability and compliance with ever-changing regulations. The wrong choice could result in delayed reimbursements, compliance issues, or revenue loss. Here are some critical factors to keep in mind during your search.
1. Experience and Expertise in the Healthcare Industry
When outsourcing medical billing and coding, look for a company with proven expertise. Experience in handling diverse medical specialties, such as cardiology, dermatology, or pediatrics, ensures the company understands the unique coding and billing challenges of your practice.
- What to Ask:
- How long have you been providing medical billing and coding services?
- Do you have experience in my specialty?
Choosing a company with a strong background in healthcare ensures your billing is handled professionally and efficiently.
2. Compliance with Industry Regulations
Medical billing and coding require adherence to strict regulatory standards like HIPAA (Health Insurance Portability and Accountability Act) and the latest ICD (International Classification of Diseases) updates. Ensure the company is compliant with these regulations to protect patient data and maintain legal compliance.
- What to Check:
- Is the company HIPAA compliant?
- Do they follow up-to-date coding standards such as ICD-10 and CPT guidelines?
3. Transparent Pricing Structure
Pricing transparency is crucial. Some companies may offer low rates but include hidden charges, while others may charge a flat percentage of collections. Ensure you understand the pricing model and what services are included.
- Questions to Ask:
- What is your pricing structure?
- Are there any additional fees for services like reporting or follow-ups?
A transparent medical billing and coding company will clearly outline all costs upfront.
4. Advanced Technology and Software
The right company should use advanced billing software and tools to ensure efficiency and accuracy. Automating processes like claim submissions and denial management can significantly improve turnaround times and reduce errors.
- Features to Look For:
- Integration with your Electronic Health Record (EHR) system
- Real-time claim tracking
- Reporting and analytics tools
Companies using cutting-edge technology often deliver better results.
5. Customized Services for Your Practice
No two healthcare practices are the same. Look for a company that offers tailored services to meet your unique needs. For instance, a small clinic may need basic billing services, while a larger hospital might require comprehensive revenue cycle management.
- Ask About:
- Scalability of services
- Customization options for your practice size and specialty
Customized solutions ensure the company can adapt as your practice grows.
6. Focus on Accuracy and Efficiency
Errors in medical billing and coding can result in denied claims, delayed payments, and compliance issues. The company you choose should prioritize accuracy to maximize reimbursements and ensure timely payments.
- Key Indicators of Accuracy:
- A low claims rejection rate
- A dedicated team for quality checks
- Regular audits and updates
Efficiency ensures that your revenue cycle runs smoothly without unnecessary interruptions.
7. Strong Communication and Customer Support
The company you choose should be responsive and accessible when you need assistance. Poor communication can lead to delays in resolving issues or misunderstandings about services.
- Look For:
- A dedicated account manager
- Multiple channels for support (email, phone, chat)
- Prompt response times
Good communication fosters a strong partnership between your practice and the billing company.
8. Positive Client References and Reviews
Reputation speaks volumes. Look for client testimonials, reviews, and case studies to gauge the company’s performance and reliability. Ask for references to hear firsthand from other practices about their experience.
- Questions to Ask:
- Can you provide references from current clients?
- Do you have case studies showcasing your success stories?
9. Comprehensive Reporting and Analytics
Regular reporting is essential to monitor the financial health of your practice. A good medical billing and coding company will provide detailed insights into claim status, reimbursement rates, and denial patterns.
- What to Expect:
- Weekly or monthly reports
- Customizable dashboards for real-time tracking
- Insights into areas of improvement
Analytics empower you to make informed decisions about your revenue cycle.
10. Commitment to Client Success
The right partner will go beyond basic services to help your practice succeed. This includes proactively addressing potential issues, offering insights to improve operations, and ensuring maximum reimbursements.
- Indicators of Commitment:
- Regular feedback sessions
- Proactive resolution of claim denials
- A focus on long-term partnerships
11. Flexible Contract Terms
Rigid contracts can be a hassle, especially if your needs change over time. Look for companies offering flexible agreements that allow you to scale services or make adjustments as needed.
- Questions to Ask:
- Can I adjust the scope of services?
- What is the cancellation policy?
12. Focus on Security and Data Protection
Medical billing and coding involve sensitive patient information. The company must have robust security measures to safeguard this data from breaches or unauthorized access.
- Security Measures to Check:
- Data encryption
- Secure servers
- Regular security audits
13. Proven Track Record with Denial Management
Denied claims are a common challenge for healthcare practices. A good billing company should have a dedicated process to identify and resolve denials efficiently.
- Questions to Ask:
- What is your approach to denial management?
- How quickly do you resolve claim issues?
14. Cost-Effective Solutions
Finally, ensure the company provides value for money. While the cost is important, focus on the quality of services and the potential for increased revenue through accurate billing and coding.
- What to Consider:
- The balance between cost and quality
- The potential ROI from outsourcing
Why Choose Apaana Healthcare?
At Apaana Healthcare, we understand the complexities of medical billing and coding. Our services are designed to drive operational excellence and deliver measurable results. Here’s why Apaana Healthcare is the ideal choice:
- Comprehensive Expertise: With years of experience, we specialize in outsourced services for health plans, including member enrollment, claims administration, medical billing and coding, and provider engagement.
- Cutting-Edge Technology: We leverage advanced tools to streamline your revenue cycle and ensure accuracy.
- Tailored Solutions: Whether you’re a small clinic or a large hospital, our services are customized to fit your unique needs.
- Cost-Effective Approach: Our solutions are designed to maximize reimbursements while reducing overhead costs.
- Proactive Support: We prioritize clear communication and timely resolution of issues to keep your practice running smoothly.
Partnering with Apaana Healthcare means entrusting your revenue cycle management to experts who care about your success.
Choosing the right medical billing and coding company is critical to the financial health of your practice. By considering the factors outlined above, you can make an informed decision that benefits your operations and bottom line. With Apaana Healthcare, you gain a trusted partner dedicated to optimizing your revenue cycle and supporting your practice’s growth.
Contact us today to learn how Apaana Healthcare can transform your medical billing and coding processes!





