In today’s fast-evolving healthcare environment, maintaining operational excellence is crucial for delivering quality care and ensuring a seamless patient experience. Two key pillars in achieving this excellence are provider enrollment and credentialing. Both play a vital role in establishing trust, maintaining compliance, and streamlining revenue cycles for healthcare facilities. Apaana’s expertise in provider enrollment and credentialing is transforming healthcare operations by enhancing the efficiency, accuracy, and speed of these processes. In this article, we’ll explore the importance of these services and how Apaana’s solutions enable healthcare providers to reach new heights of operational excellence.
Understanding Provider Enrollment and Credentialing
Provider Enrollment is the process of registering healthcare providers with insurance companies, enabling them to bill and receive reimbursements for their services. Without enrollment, providers cannot submit claims to insurers, making it essential for a successful revenue cycle.
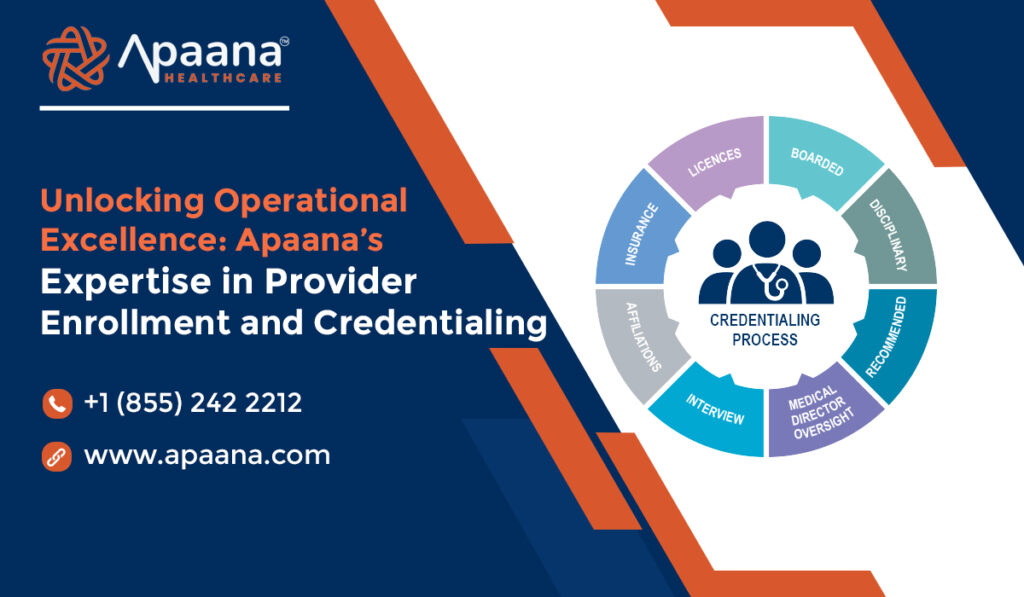
Credentialing is the process of verifying a provider’s qualifications, including education, training, licensing, and professional history. This rigorous process assures patients, insurers, and healthcare facilities that providers meet high standards of quality and competence.
Together, enrollment and credentialing form the foundation of trust and financial viability for healthcare practices. However, these processes can be challenging and time-consuming, particularly for multi-specialty practices or providers operating across various states. Apaana’s expertise in these areas simplifies the process, enabling healthcare organizations to focus on what matters most—patient care.
The Challenges of Provider Enrollment and Credentialing
Both provider enrollment and credentialing come with unique challenges that can slow down the onboarding process, delay revenue, and expose healthcare providers to compliance risks:
Complex and Lengthy Processes: Each insurer has unique requirements, leading to complex paperwork and long processing times.
Credentialing can take weeks or even months, causing delays in providers’ ability to start billing.Frequent Regulatory Changes: Healthcare regulations and insurance policies change frequently, making it challenging to stay compliant without dedicated expertise.
High Risk of Denials: Incorrect or incomplete enrollment applications often result in denials or delays, which can disrupt cash flow and strain operations.
Resource-Intensive Requirements: Credentialing and enrollment require careful attention to detail, which can be labor-intensive and time-consuming for in-house teams.
Apaana addresses these challenges head-on, offering customized solutions that enable healthcare providers to streamline operations, reduce risks, and improve their bottom line.
How Apaana Unlocks Operational Excellence
Apaana’s credentialing and provider enrollment services are designed to optimize these critical processes, enhancing operational efficiency and minimizing the burden on healthcare staff. Here’s how Apaana’s solutions unlock operational excellence:
1. Streamlined Process Management
Apaana simplifies each step of the enrollment and credentialing process. By handling everything from documentation collection to primary source verification, Apaana accelerates the time required to complete applications, reducing onboarding times and enabling providers to start billing sooner.
2. Regulatory Expertise
Apaana stays up-to-date with the latest regulatory changes and payer requirements, ensuring all enrollment and credentialing activities comply with current standards. This reduces the risk of costly errors, denials, and compliance issues, protecting healthcare organizations from potential legal complications and financial losses.
3. Efficient Denial Management
With expert knowledge of payer requirements and a meticulous approach to application submissions, Apaana reduces the risk of denials by ensuring all documentation is accurate and complete. In cases where denials do occur, Apaana’s team manages resubmissions, helping providers resolve issues quickly and maintain a steady cash flow.
4. Advanced Data Management
Apaana uses cutting-edge technology to manage data, track application statuses, and ensure timely renewals for providers. This not only reduces administrative burden but also enables healthcare organizations to monitor credentialing and enrollment data in real time, making it easier to maintain up-to-date records and meet ongoing compliance requirements.
5. Customized Solutions for Diverse Needs
Every healthcare organization has unique needs, and Apaana provides tailored credentialing and enrollment solutions that address the specific requirements of each client. Whether it’s multi-state licensing, specialty-specific requirements, or rapid enrollment for new providers, Apaana adapts to deliver efficient, cost-effective solutions.
Benefits of Apaana’s Provider Enrollment and Credentialing Services
Apaana’s expertise in provider enrollment and credentialing offers several distinct benefits for healthcare providers:
Reduced Onboarding Time: With a streamlined approach to enrollment and credentialing, providers can begin seeing patients and billing insurers faster, minimizing revenue disruptions.
Improved Cash Flow: Efficient enrollment with multiple payers enables providers to expand their patient base and ensure consistent reimbursements, optimizing revenue cycles.
Enhanced Compliance and Security: Apaana’s focus on compliance reduces the risk of regulatory fines and enhances the security of provider data through stringent verification processes.
Operational Efficiency: Apaana’s services free up healthcare teams to focus on clinical and operational responsibilities, enhancing productivity and minimizing administrative workloads.
Patient Trust and Safety: By verifying each provider’s credentials thoroughly, Apaana ensures that patients receive care from qualified, trusted professionals, enhancing the facility’s reputation and patient confidence.
Why Choose Apaana?
Apaana stands out in the field of provider enrollment and credentialing through its commitment to operational excellence, accuracy, and client-focused solutions. Apaana’s dedicated team of experts brings a wealth of experience and a proactive approach to every client engagement, ensuring that each healthcare provider receives the individualized attention they need.
Apaana is not just a service provider; it’s a partner in enhancing healthcare operations. By helping organizations stay compliant, manage payer relationships, and reduce credentialing-related delays, Apaana enables healthcare providers to deliver quality care with fewer administrative hassles.
Conclusion
In the healthcare industry, operational excellence is key to providing high-quality patient care and maintaining a stable revenue stream. Apaana’s expertise in provider enrollment and credentialing allows healthcare organizations to optimize their revenue cycle, maintain regulatory compliance, and build patient trust.
With Apaana as a partner, healthcare providers can focus on their core mission—delivering exceptional care to their patients—while leaving the complexities of enrollment and credentialing in expert hands.
By choosing Apaana, healthcare providers gain a strategic advantage in achieving operational excellence, reducing costs, and enhancing patient satisfaction. As the demands of healthcare continue to grow, partnering with a trusted credentialing and enrollment consultant like Apaana ensures your practice is prepared, compliant, and positioned for success.