In the ever-evolving healthcare landscape, healthcare providers are not only expected to deliver high-quality care but also to navigate the complex world of administrative tasks. One of the most critical administrative processes is credentialing and enrollment. This process ensures that healthcare providers are recognized and reimbursed by insurance companies and other payers for the services they provide. However, this process can be time-consuming and complex.
In this blog, we will explore what credentialing and enrollment services are, why they are essential, and how partnering with experts can save your practice time and money.
What Is Credentialing?

Credentialing refers to the process of verifying the qualifications and credentials of a healthcare provider to ensure they meet the standards of the medical profession. It involves validating education, training, licensure, experience, and professional standing.
Some key components of credentialing include:
- Verification of Education: Ensuring the provider has completed the necessary education and training.
- Verification of Licensure: Confirming that the provider holds the appropriate licenses for their field of practice.
- Verification of Experience: Assessing previous work experience, certifications, and any specialties the provider holds.
Credentialing is essential for patient safety and maintaining the integrity of the healthcare system. It is typically required by hospitals, insurance companies, and various healthcare facilities before a provider can deliver care or bill for services.
What Is Enrollment?
Once a healthcare provider has been credentialed, the next step is enrollment. Enrollment is the process of a provider being added to the network of an insurance company or payer. This step ensures that the provider is recognized as an “in-network” provider, allowing them to bill and receive reimbursements for services rendered to patients with specific insurance coverage.
The enrollment process involves:
- Completing payer-specific applications
- Submitting required documentation (licenses, certifications, etc.)
- Waiting for approval, which can take several weeks to months depending on the payer and complexity of the application.
In short, credentialing verifies a provider’s qualifications, while enrollment places the provider in the payer’s network, enabling them to receive payments for their services.
The Importance of Credentialing and Enrollment Services
Without credentialing and enrollment, healthcare providers face the risk of delayed or denied reimbursements. They may also be excluded from insurance networks, limiting the number of patients they can serve. Effective credentialing and enrollment are essential for:
- Ensuring Compliance: It ensures that providers meet industry standards and are compliant with healthcare regulations.
- Timely Reimbursement: Providers cannot bill insurance companies without being enrolled in their networks.
- Avoiding Legal Issues: Proper credentialing helps avoid legal risks associated with unverified or unlicensed practice.
- Building Patient Trust: Being enrolled and credentialed demonstrates professionalism and commitment to quality care.
Challenges in Credentialing and Enrollment
The process of credentialing and enrollment is fraught with challenges, especially for new providers or smaller practices. Some common challenges include:
- Lengthy Process: Credentialing and enrollment can take anywhere from 60 to 180 days, depending on the payer.
- Paperwork Overload: Managing extensive documentation, forms, and payer-specific requirements can be overwhelming.
- Frequent Updates: Credentialing information must be regularly updated to maintain network participation.
- Complex Regulations: Providers must navigate a maze of regulations from federal, state, and payer-specific guidelines.
Benefits of Outsourcing Credentialing and Enrollment Services
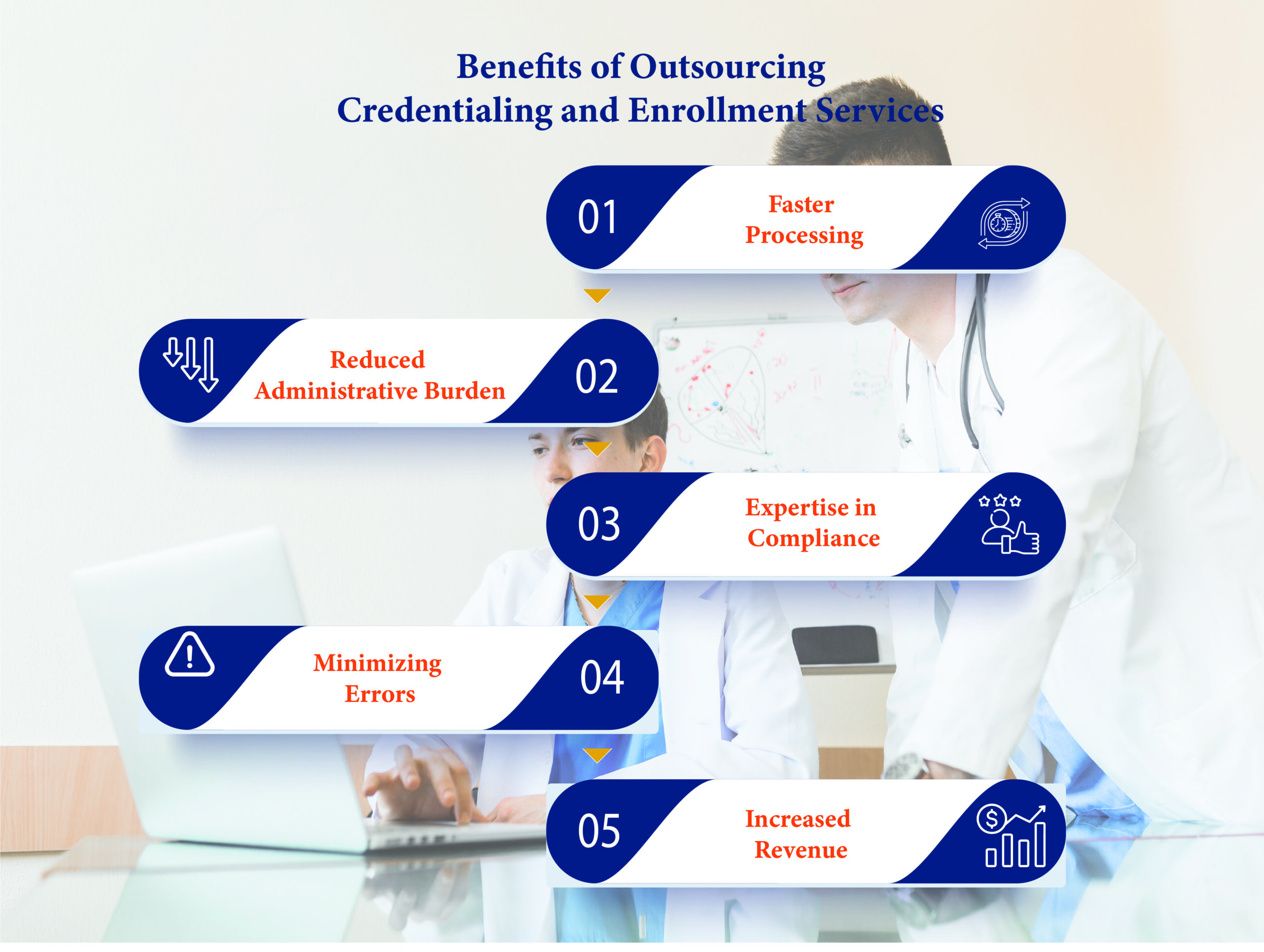
Given the complexity of credentialing and enrollment, many healthcare providers opt to outsource these tasks to credentialing service providers. Here are some key benefits of outsourcing:
- Faster Processing: Credentialing service providers specialize in navigating the complex application process, reducing delays and speeding up approvals.
- Reduced Administrative Burden: By outsourcing, healthcare practices can free up staff time, allowing them to focus on patient care rather than administrative tasks.
- Expertise in Compliance: Credentialing experts stay up to date with the latest regulatory changes, ensuring that your practice remains compliant with payer and government regulations.
- Minimizing Errors: Credentialing professionals are experienced in completing paperwork and can help avoid common errors that may lead to delays or denials.
- Increased Revenue: By ensuring quick and accurate enrollment, providers can start billing and receiving payments sooner, improving cash flow.
Final Thoughts
Credentialing and enrollment services are essential for the smooth operation of any healthcare practice. With proper credentialing, healthcare providers can maintain compliance, ensure patient safety, and receive timely reimbursements. Although the process is complex, outsourcing these services to a specialized team can save time, reduce errors, and allow healthcare providers to focus on what matters most—delivering high-quality patient care.
If you are a healthcare provider looking to streamline your credentialing and enrollment process, partnering with a professional service provider can be a game-changer for your practice.
Why Choose Apaana Healthcare for Credentialing and Enrollment Services?
At Apaana Healthcare, we specialize in managing the complexities of credentialing and enrollment for healthcare providers. With our expert team, we ensure quick turnaround times, accurate documentation, and hassle-free processes so you can focus on growing your practice and delivering exceptional care.
Let us handle the paperwork while you focus on what you do best—caring for your patients.
Feel free to reach out to us today for a consultation and see how we can support your practice’s success!





